Have you put off your colonoscopy?
Screening test can locate, treat cancers that are showing up in younger people
BY AMBER SMITH
Many patients who are diagnosed with colon or rectal cancers have no symptoms. Some have vague complaints of abdominal pain, changes in bowel habits or blood in the stool, reports Upstate colorectal surgeon Kristina Go, MD.
Colorectal cancer is the second leading cause of cancer death in the United States. When it’s caught early, it can often be cured, she says.
Rates of colorectal cancer in people under 50 have doubled since 1990. That’s why men and women are now recommended to begin screening at age 45 — and even earlier if they have a family history of the disease.
Go answers five common questions related to colonoscopy, below:
Q: Why must the bowels be thoroughly emptied?
A: I really want to look at the inner lining of the colon, called the mucosa. In order for a patient to have a clean colon, they literally need to flush out any kind of solid and liquid waste so that we can see the clean inside area.
Q: What does the inside of the gastrointestinal, or GI, tract look like?
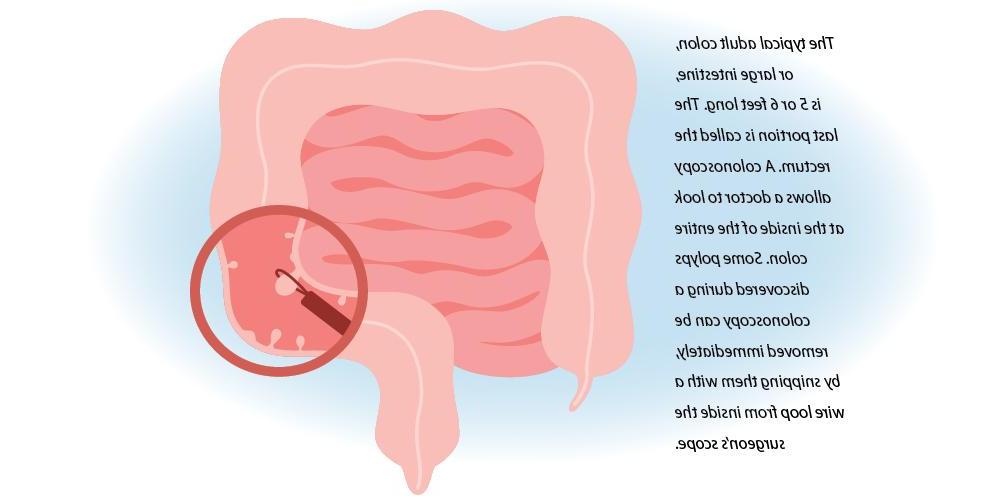
A: In a normal colon, the inside lining is nice and smooth, and you can see the underlying blood vessels, and it can even look pretty shiny during a colonoscopy.
When I see a polyp, they usually look like little bumps, or they can almost look like little mushrooms. Polyps are abnormal clumps of cells. They can have the potential to grow into a cancer — which is why we get very excited about doing colonoscopies, to prevent them from turning into cancer — but you have some polyps that never turn into a cancer.
Experience and expertise can let us know which polyps look more suspicious.
Q: How fast does food move through?
A: It depends on the individual, and sometimes it can even be variable within the same person. On average, in a non-constipated patient, that transit time solely through the colon can take about 30 to 40 hours, and even going to 72 to 100 hours can still be considered normal.
It can be variable in the same patient, based on how much physical activity they’ve had in the day, what kinds of foods they’ve had and whether they were more processed foods or more fluid and more whole grains.
And from patient to patient, it can also depend on any kind of medicines or underlying medical conditions they might have.
Q: Can the bowel prep (the laxative the patient must drink) be more palatable?
A: The osmotic laxatives doctors prescribe before colonoscopies are designed to hydrate and soften stool to unblock your system without harsh gastrointestinal side effects. Most patients are not fond of the taste, especially since they may have to swallow 64 ounces of prep fluid.
To help you drink that prep: Place your prep on ice. Drink it through a straw. Suck on lemon slices or sugar-free menthol candy to decrease nausea.
In the week prior to your screening test, avoid high-fiber foods — no leafy green vegetables, no beans, no fiber supplements — exactly the opposite advice I tell my patients for their colon health. After the colonoscopy, you should return to a high-fiber diet.
Q: Are there alternatives to a colonoscopy?
A: Stool-based tests that look for blood in your GI tract are pretty good at detecting cancers, but they provide no information about polyps. If you get a positive result from these tests, you’ll need a colonoscopy.
“Virtual” colonoscopy is a test that requires the same bowel prep. Then, instead of a camera scope in your colon, your colon is inflated with air, and you’re asked to move into several positions while computerized tomography images (CT, or CAT, scans) are made. Any polyps that are detected cannot be removed using this method, and if the doctor sees anything of concern, you’ll need a colonoscopy.
(Click here to hear Kristina Go talk about how colorectal cancer is diagnosed and treated in this episode of Upstate's "The Informed Patient" podcast.)
This article appears in the summer 2023 issue of Cancer Care magazine.